Digital twin: how AI is helping with diabetes and obesity
Twin Health’s digital twin isn’t sci-fi-it’s a working program combining wearable sensors, a mobile app, and AI that simulates human metabolism. In a clinical study, participants with type 2 diabetes were more likely to hit A1C levels below 6.5% after 12 months while also reducing their medication intake. The program has also become a go-to solution for employers looking to curb rising costs associated with GLP‑1 drugs like Ozempic.
How the digital twin works
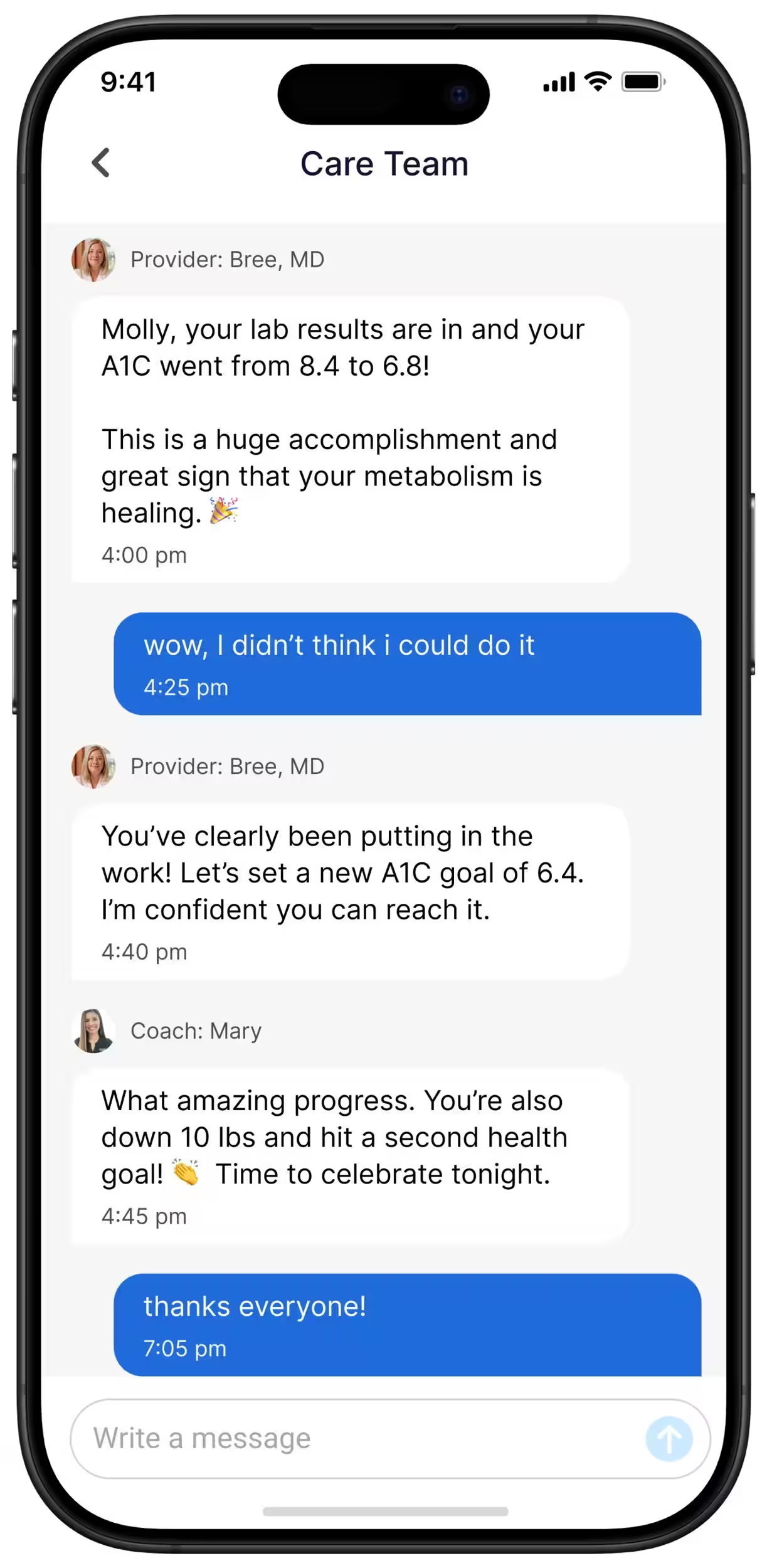
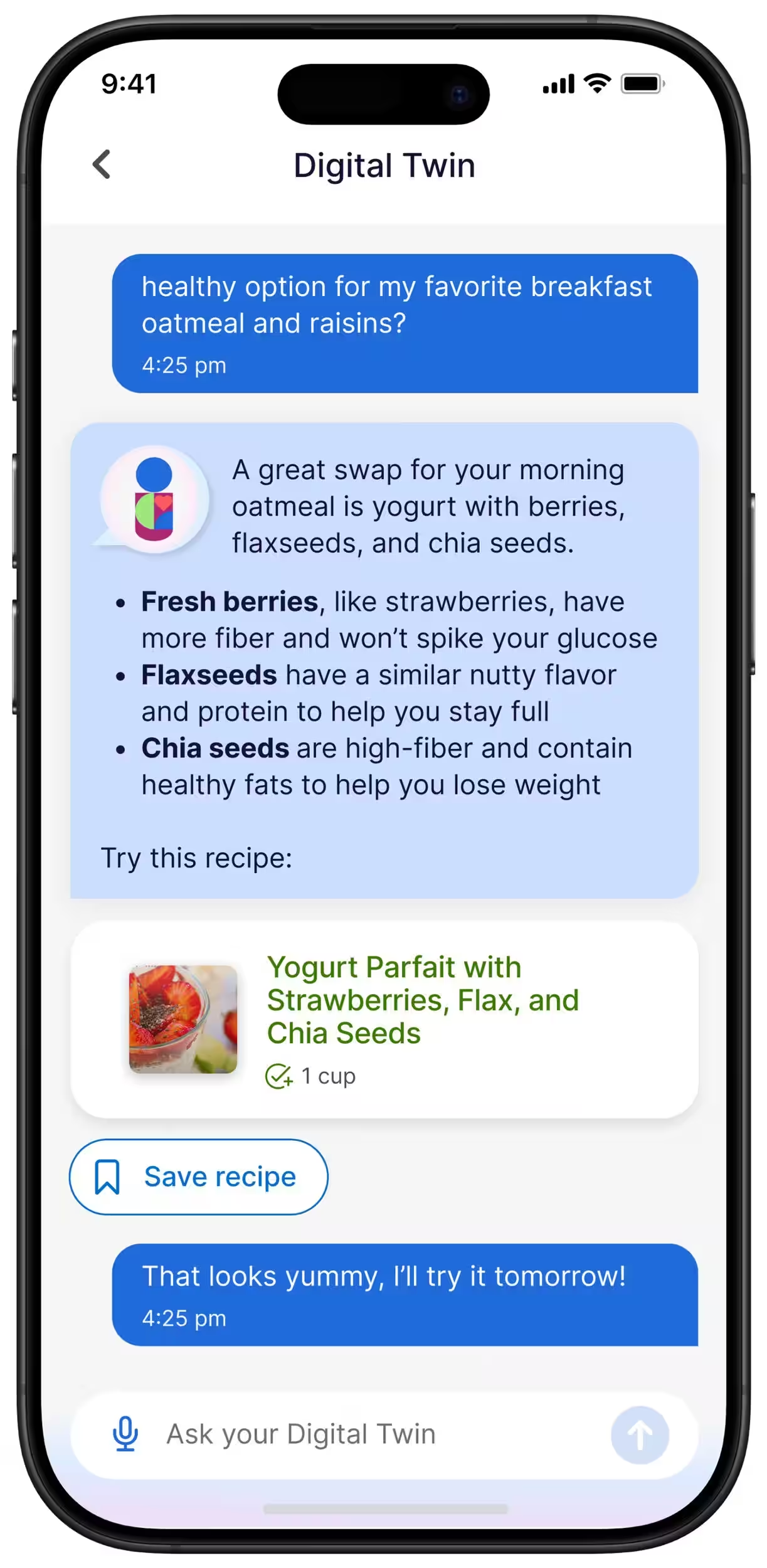
Twin Health collects a flood of biometric data via a continuous glucose monitor, blood pressure cuff, smart scales, and fitness tracker. All measurements – glucose, weight, blood pressure, sleep, activity, and stress levels – feed into a single app, where a predictive model builds a virtual metabolic profile of the user. By logging meals, the app forecasts blood sugar responses and offers real-time personalized advice, with access to live coaches for extra support.
- What the program provides: continuous glucose monitor, blood pressure cuff, smart scales, fitness tracker.
- What’s analyzed: glucose, weight, blood pressure, sleep, activity, stress, nutrition.
- What the model does: predicts sugar response to food, recommends portions, food combinations, and activity levels.
- How companies pay: Twin Health gets compensated only when certain clinical milestones are met (A1C reduction, weight loss, less medication).
Clinical study results
A Cleveland Clinic study with 150 type 2 diabetes patients showed striking outcomes: after 12 months, 71% of Twin Health users achieved an A1C under 6.5% with fewer medications, compared to just 2% in the control group. The Twin group also lost an average of 8.6% body weight versus 4.6% for controls. Before the study, 41% of Twin participants used GLP‑1 drugs; by the end, only 6% did. Meanwhile, GLP‑1 usage rose from 52% to 63% in the control arm.
The findings, published in the New England Journal of Medicine Catalyst, add weight to digital programs that aim not just to control metrics but to reduce medication burden.
“When I started the program, I could barely walk a mile: my back hurt, my knee hurt. Now I cover six and a half miles every morning.”
Rodney Buckley, former firefighter, mayor of Third Lake, Illinois
Why employers are interested
The rising popularity of GLP‑1 drugs like Novo Nordisk’s Ozempic has driven healthcare costs up sharply-around $1,000 to $1,500 a month per person. This hits companies’ bottom lines hard, prompting some employers to look for alternatives. Result-based programs like Twin Health make sense, with firms like Blackstone already reporting drug cost savings alongside improved employee health.
The market has similar options: Virta Health targets diabetes remission through a remote clinical program, while Omada and Noom focus on behavior change and weight loss. Twin stands out by zeroing in on continuous biometric data and tailoring its model to each individual’s metabolism.
Limitations and risks
Programs relying on constant monitoring come with psychological downsides: daily weigh-ins and measurements can be stressful or discouraging for some. Patients already doing well on GLP‑1 drugs may be reluctant to stop them, especially if previous lifestyle changes didn’t work.
From a privacy standpoint, employers only receive aggregated reports on participation and outcomes. Twin Health says it complies with HIPAA and state privacy laws and undergoes third-party security audits. Still, concerns remain about how health data might be interpreted in workplace programs tied to incentives or employee retention.
What’s next
The trend is clear: digital services combining wearables and AI are becoming valuable tools for reducing medication costs and scaling preventive care. The big questions are whether these programs can thrive outside corporate benefits, how result-based payment models will evolve, and how to balance helpful feedback with overreach into personal data.
If digital twins truly enable patients to lower doses or ditch expensive drugs without losing disease control, it could reshape how pharma companies, insurers, and employers calculate value. But widespread adoption will require more long-term studies, transparent privacy standards, and a willingness among clinicians to integrate these tools into everyday practice.